Anemia During Pregnancy: Healthy Mother & Baby
Anemia During Pregnancy: Healthy Mother & Baby
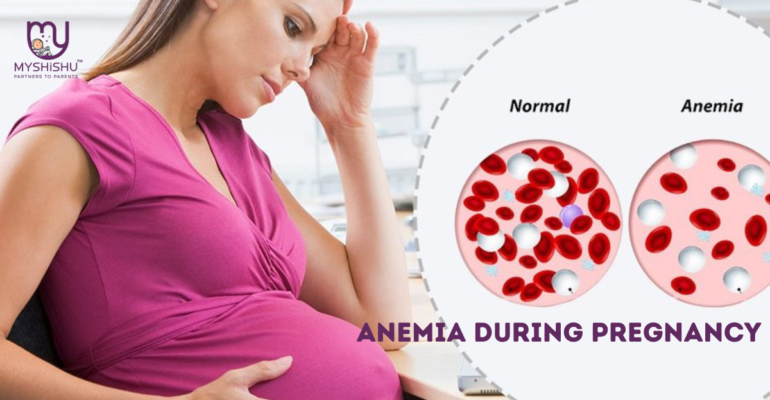
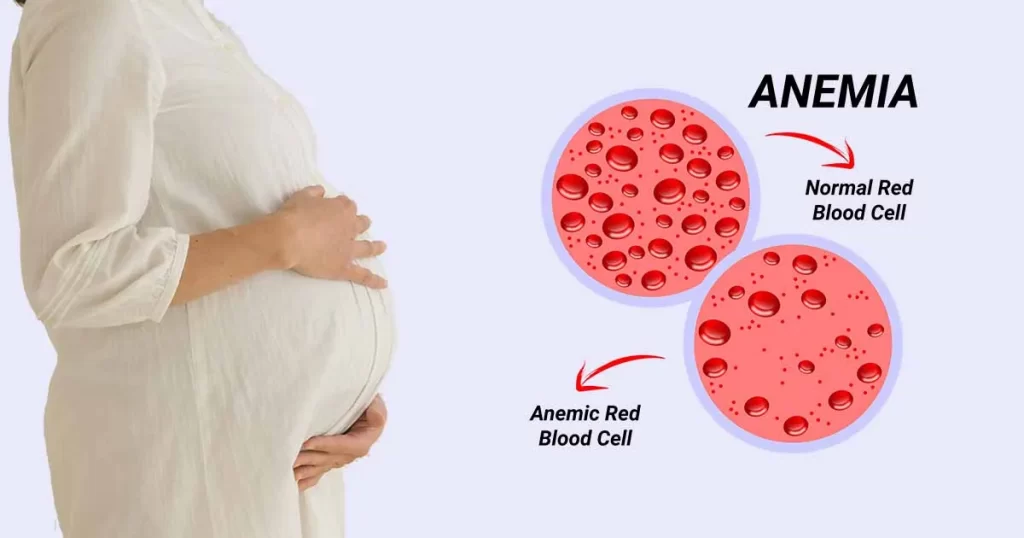
Anemia occurs when there is a deficiency of red blood cells or haemoglobin in the blood, leading to reduced oxygen-carrying capacity. In this blog, we will explore the causes, symptoms, and management of anemia during pregnancy, emphasizing the importance of early detection and proper intervention for the well-being of both the mother and the developing baby.
Table of Contents
- Introduction
- Types of Anemia Affecting During Pregnancy
- Causes of Anemia during pregnancy
- Is it normal to be anemia during pregnancy?
- How does Anemia affect your body during pregnancy?
- Can Anemia during pregnancy cause miscarriage?
- Symptoms of Anemia during pregnancy
- Diagnosis of Anemia during pregnancy
- Prevention & Treatment
- FAQs
Introduction
When your body doesn’t have enough red blood cells to distribute oxygen throughout it, you have anemia. Your body can’t work correctly if it doesn’t get enough oxygen from the blood. Anemic is the term used to describe someone who suffers anemia when pregnant.
An essential protein known as haemoglobin is found in red blood cells (RBCs). To help your red blood cells transport oxygen from your lungs to your body, this protein stores oxygen. It also helps transfer carbon dioxide from your body to your lungs so you may breathe it out.
Your body needs a steady supply of vitamins and iron to make haemoglobin and red blood cells. Your body cannot adequately manufacture enough haemoglobin to transport oxygen to your organs without that supply. It’s typical for women to develop anemia.
Types of Anemia Affecting During Pregnancy
During pregnancy, several types of anemia can occur, each with its distinct causes and characteristics. The most common types include:
- Iron-Deficiency Anemia:
- This is the most prevalent type of anemia during pregnancy. Iron is essential for the production of hemoglobin, the oxygen-carrying protein in red blood cells. In pregnancy, the demand for iron increases significantly to support the growing fetus. If the mother’s iron intake is insufficient, it can lead to a decrease in hemoglobin levels, resulting in iron-deficiency anemia.
- Folate-Deficiency Anemia:
- Folate, also known as vitamin B9, is crucial for the synthesis of DNA and red blood cells. A deficiency in folate can lead to the production of larger-than-normal red blood cells (megaloblasts), causing folate-deficiency anemia. Adequate folate intake is particularly important in early pregnancy to prevent neural tube defects in the developing fetus.
- Vitamin B12 Deficiency Anemia:
- Vitamin B12 is essential for the formation of red blood cells and the proper functioning of the nervous system. A deficiency in vitamin B12 can result in pernicious anemia, characterized by abnormally large and fragile red blood cells. This type of anemia is less common but can occur in individuals with poor dietary intake of B12 or malabsorption issues.
- Hemolytic Anemia:
- Hemolytic anemia is characterized by the destruction of red blood cells at a rate faster than the body can replace them. It can be caused by various factors, including inherited conditions, autoimmune disorders, or certain infections. While less common, hemolytic anemia can impact pregnant women, and its management may require specialized care.
- Sickle Cell Anemia:
- Sickle cell anemia is an inherited blood disorder where the shape of red blood cells becomes abnormal, leading to increased fragility and reduced oxygen-carrying capacity. Pregnant women with sickle cell anemia may face additional challenges due to the impact of the condition on blood circulation.
- Thalassemia:
- Thalassemia is a group of inherited blood disorders that affect the production of hemoglobin. Depending on the severity of thalassemia, pregnant women may experience varying degrees of anemia. The management of thalassemia during pregnancy often requires close collaboration between obstetricians and hematologists.
Causes of Anemia during pregnancy
Several factors contribute to the development of anemia during pregnancy. Understanding these causes is essential for both expectant mothers and healthcare providers to implement effective preventive measures and interventions. The primary causes include:
- Iron Deficiency:
- Iron is a vital component of hemoglobin, and its deficiency is a leading cause of anemia. During pregnancy, the demand for iron increases to support the growing fetus and placenta.
- Folate Deficiency:
- Folate, also known as vitamin B9, is crucial for the production of red blood cells. Inadequate intake of folate during pregnancy can contribute to anemia.
- Vitamin B12 Deficiency:
- Vitamin B12 plays a role in red blood cell formation and neurological function. A deficiency in this vitamin can lead to anemia and potential developmental issues for the baby.
- Chronic Diseases:
- Underlying chronic conditions such as inflammatory diseases, chronic kidney disease, or autoimmune disorders can contribute to anemia during pregnancy.
- Multiple Pregnancies:
- Women carrying twins or higher-order multiples may be at an increased risk of developing anemia due to the higher demands on their bodies.
- Teenage Pregnancy:
- Adolescent mothers may be more prone to anemia due to their bodies still growing and developing, requiring additional nutrients.
- Poor Diet:
- Inadequate intake of iron-rich foods, folate, and vitamin B12 can contribute to anemia. Diets lacking essential nutrients can result in decreased red blood cell production.
Is it normal to be anemia during pregnancy?
Yes. Mild anemia is usual during pregnancy since blood volume increases. Pregnant women in underdeveloped nations often experience iron insufficiency; as many as 52% of them do not acquire adequate iron during their pregnancy. Severe anemia is uncommon.
To safeguard your health and the welfare of the fetus, treatment is necessary for both mild and severe anemia.
How does Anemia affect your body during pregnancy?
Untreated or severe anemia during pregnancy can lead to various complications, affecting both the mother and the developing baby. Some potential complications include:
- Preterm Birth:
- Anemia women may have an increased risk of delivering prematurely, which can pose health risks for the newborn.
- Low Birth Weight:
- Inadequate oxygen supply to the fetus can result in low birth weight, impacting the baby’s overall health and development.
- Postpartum Depression:
- Anemia may contribute to postpartum depression, affecting the mother’s emotional well-being after childbirth.
- Fatigue and Weakness:
- Severe anemia can lead to extreme fatigue and weakness, hindering the mother’s ability to care for herself and her newborn.
- Developmental Delays in the Baby:
- Insufficient oxygen delivery to the developing fetus may lead to developmental delays or cognitive impairments.
Can Anemia during pregnancy cause miscarriage?
While mild or moderate anemia is generally not associated with an increased risk of miscarriage, severe anemia during pregnancy can potentially contribute to complications that may affect the pregnancy outcome. It’s important to understand the factors involved and how anemia might be linked to pregnancy complications:
- Reduced Oxygen Supply:
- Severe anemia means there is a significant reduction in the number of red blood cells or hemoglobin in the blood. This can lead to reduced oxygen-carrying capacity, potentially affecting the oxygen supply to the developing fetus.
- Preterm Birth:
- Severe anemia has been linked to an increased risk of preterm birth. Preterm birth, especially very early preterm birth, is associated with a higher risk of complications for the newborn, including developmental issues and low birth weight.
- Low Birth Weight:
- In cases where anemia is severe and long-standing, it may contribute to low birth weight in newborns. Low birth weight can increase the risk of health problems for the baby.
- Fetal Distress:
- In severe cases of anemia, the fetus may experience distress due to inadequate oxygen supply. This can potentially lead to complications during labor and delivery.
It’s crucial to note that the risk of these complications is primarily associated with severe anemia, and moderate or mild anemia is generally less likely to lead to adverse outcomes.
Symptoms of Anemia during pregnancy
Recognizing the symptoms of anemia is crucial for early detection and appropriate management. Common signs of anemia during pregnancy include:
- Fatigue:
- Persistent fatigue and weakness are common symptoms of anemia, as the body struggles to supply enough oxygen to tissues and organs.
- Pale Skin and Nail Beds:
- Anemic individuals may exhibit paleness in their skin and nail beds due to reduced blood flow and oxygenation.
- Shortness of Breath:
- Insufficient oxygen-carrying capacity may lead to shortness of breath, especially during physical exertion.
- Dizziness or Lightheadedness:
- Inadequate oxygen supply to the brain can cause dizziness or lightheadedness, particularly when standing up quickly.
- Rapid Heartbeat:
- The heart may beat faster to compensate for the reduced oxygen-carrying capacity, resulting in a rapid heartbeat.
- Cold Hands and Feet:
- Poor circulation can cause extremities to feel cold, even in warm environments.
- Difficulty Concentrating:
- Anemia may affect cognitive function, leading to difficulty concentrating or mental fogginess.
Diagnosis of Anemia during pregnancy
The diagnosis of anemia during pregnancy involves a combination of medical history, physical examinations, and laboratory tests. Healthcare providers routinely monitor for anemia during prenatal care to detect and address any deficiencies early on. Here are the key steps involved in diagnosing anemia during pregnancy:
- Medical History:
- The healthcare provider will begin by taking a thorough medical history, including details about the woman’s diet, any known pre-existing conditions, previous pregnancies, and any history of anemia or related disorders. Information about the use of supplements or medications will also be important.
- Physical Examination:
- A physical examination may reveal signs of anemia, such as pale skin, pale mucous membranes (inside the mouth), and a rapid heartbeat. The healthcare provider will assess general health and well-being, looking for any visible signs or symptoms of anemia.
- Blood Tests:
- Blood tests are essential for a definitive diagnosis of anemia. The following blood tests are commonly performed:
- Complete Blood Count (CBC): This test measures the number and types of blood cells, including red blood cells, white blood cells, and platelets. Hemoglobin and hematocrit levels are crucial components of the CBC and provide information about the oxygen-carrying capacity of the blood.
- Peripheral Blood Smear: A blood smear may be examined under a microscope to assess the size and shape of red blood cells, helping to identify specific types of anemia.
- Serum Ferritin Level: Ferritin is a protein that stores iron. Low levels of serum ferritin indicate an iron deficiency, a common cause of anemia.
- Serum Folate and Vitamin B12 Levels: These tests help identify deficiencies in folate or vitamin B12, which can contribute to specific types of anemia.
- Blood tests are essential for a definitive diagnosis of anemia. The following blood tests are commonly performed:
- Additional Tests:
- Depending on the results of initial tests and the clinical presentation, additional tests may be conducted to identify the specific type and cause of anemia. These may include tests for hemoglobin electrophoresis, markers of inflammation, or tests to assess the function of organs that play a role in red blood cell production.
- Evaluation of Underlying Causes:
- If anemia is diagnosed, the healthcare provider will investigate the underlying causes. This may involve additional tests to assess for conditions such as chronic diseases, thalassemia, sickle cell disease, or other factors contributing to the anemia.
Once the diagnosis is confirmed, the healthcare provider will develop a treatment plan tailored to the specific type and severity of anemia. This may include dietary recommendations, iron or other supplements, and close monitoring throughout the remainder of the pregnancy.
Prevention & Treatment of Anemia during pregnancy
To promote a healthy pregnancy and prevent complications associated with anemia, proactive measures should be taken. Here are some strategies for prevention and management:
- Iron-Rich Diet:
- Consuming a well-balanced diet rich in iron is essential. Iron-rich foods include lean meats, poultry, fish, beans, lentils, spinach, and fortified cereals.
- Supplementation:
- Prenatal vitamins containing iron, folate, and vitamin B12 are commonly recommended during pregnancy to supplement dietary intake.
- Regular Monitoring:
- Healthcare providers should regularly monitor the hemoglobin levels of pregnant women during prenatal check-ups to detect and address anemia early.
- Folate and Vitamin B12 Supplements:
- If a woman is at risk of deficiencies in folate or vitamin B12, supplementation may be recommended to support red blood cell production.
- Manage Underlying Conditions:
- Effective management of chronic diseases and conditions that contribute to anemia is crucial for a healthy pregnancy.
- Avoidance of Iron Inhibitors:
- Some substances, such as caffeine and calcium, can inhibit iron absorption. Pregnant women should be mindful of their consumption of these substances.
- Hydration:
- Staying well-hydrated is important for maintaining blood volume and preventing dehydration, which can exacerbate anemia.
- Rest and Sleep:
- Adequate rest and sleep are essential for the well-being of pregnant women. Managing fatigue through proper rest can help alleviate symptoms of anemia.
Anemia during pregnancy is a common concern that requires attention and proactive management. By understanding the causes, symptoms, and potential complications associated with anemia, expectant mothers and healthcare providers can work together to implement effective preventive measures and interventions. Early detection, proper nutrition, and regular monitoring are key components of a comprehensive approach to managing anemia during pregnancy. Ensuring the well-being of both the mother and the developing baby is paramount, and addressing anemia contributes to a healthier pregnancy and a positive birth outcome. Pregnant women are encouraged to communicate openly with their healthcare providers, adhere to recommended prenatal care, and make lifestyle choices that promote optimal maternal and fetal health.
Frequently Asked Questions (FAQs)
1. What is anemia, and how does it relate to pregnancy?
- Anemia is a condition characterized by a deficiency of red blood cells or hemoglobin in the blood. During pregnancy, the body’s demand for blood increases, and if this demand is not met due to factors such as nutritional deficiencies, anemia can occur.
2. What are the common causes of anemia during pregnancy?
- The most common causes of anemia during pregnancy include iron deficiency, folate deficiency, vitamin B12 deficiency, chronic diseases, multiple pregnancies, teenage pregnancy, and poor dietary intake.
3. How is anemia diagnosed during pregnancy?
- Anemia is diagnosed through blood tests, including a complete blood count (CBC), peripheral blood smear, and measurement of serum ferritin, folate, and vitamin B12 levels. These tests help determine the type and severity of anemia.
4. What are the symptoms of anemia during pregnancy?
- Symptoms may include fatigue, weakness, pale skin and nail beds, shortness of breath, dizziness or lightheadedness, rapid heartbeat, cold hands and feet, and difficulty concentrating.
5. Can anemia during pregnancy lead to complications?
- Severe anemia, if left untreated, can contribute to complications such as preterm birth, low birth weight, and developmental delays in the baby. It may also impact the mother’s well-being.
6. How can anemia during pregnancy be prevented?
- Prevention strategies include maintaining a balanced diet rich in iron, folate, and vitamin B12, taking prenatal vitamins, and undergoing regular prenatal check-ups for early detection and management.
7. What is the treatment for anemia during pregnancy?
- Treatment options may include dietary changes, iron supplements, and, in some cases, vitamin B12 or folate supplements. The specific treatment plan depends on the type and severity of anemia.
8. Is it safe to take iron supplements during pregnancy?
- Yes, iron supplements are commonly recommended during pregnancy, especially for women with iron-deficiency anemia. It’s important to follow healthcare provider recommendations regarding dosage and timing.
9. Can anemia during pregnancy be a sign of an underlying health condition?
- Yes, anemia can sometimes be a symptom of underlying conditions such as chronic diseases, thalassemia, or autoimmune disorders. Further tests may be conducted to identify any contributing factors.
10. How often should I have my hemoglobin levels checked during pregnancy?
- Hemoglobin levels are typically checked during the first prenatal visit and periodically throughout the pregnancy, as recommended by your healthcare provider. The frequency may depend on individual risk factors and the presence of symptoms.