Endometrial Hyperplasia Demystified: A Comprehensive Overview
Endometrial Hyperplasia Demystified: A Comprehensive Overview
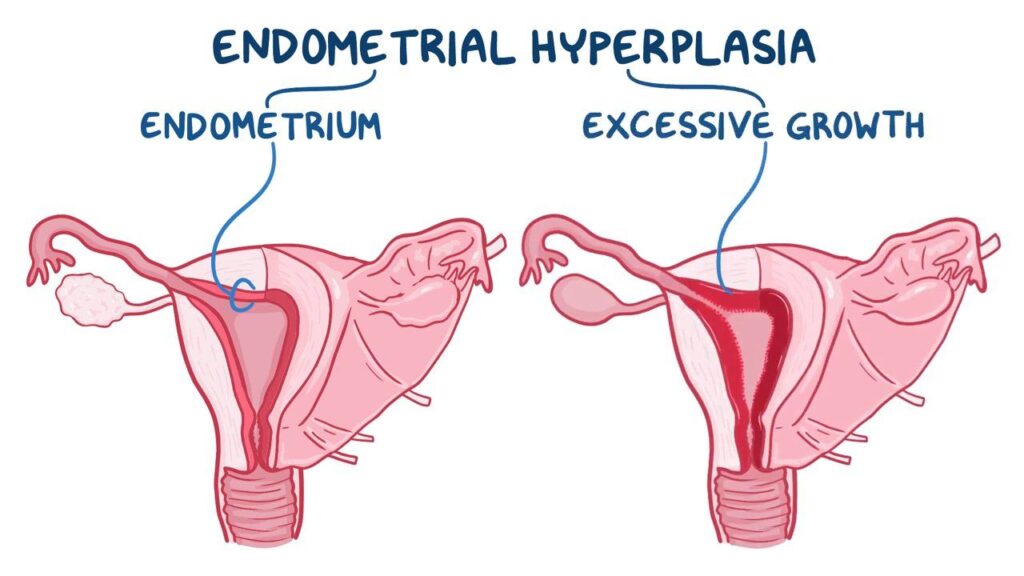
Endometrial hyperplasia is a condition that affects the lining of the uterus, causing an overgrowth of cells. While not cancerous itself, untreated or undiagnosed endometrial hyperplasia can increase the risk of developing endometrial cancer. In this comprehensive blog, we will delve into the intricacies of endometrial hyperplasia, exploring its definition, causes, symptoms, diagnosis, treatment options, and the importance of proactive management.
Table of Contents
Introduction
Endometrial hyperplasia is a precancerous condition in which there is an irregular thickening of the uterine lining. This may cause uncomfortable symptoms for women, including heavy menstrual periods, postmenopausal bleeding, and anemia due to the excess bleeding. It is a condition in which the lining of your womb becomes too thick. In some women, this can lead to cancer of the uterus.
Endometrial hyperplasia is most common among women in their 50s and 60s who have experienced menopause. It may also occur in women who are in perimenopause, a transitional state during which women still have their menstrual periods but on an irregular basis.
Understanding Endometrial Hyperplasia
- Definition and Basics: Endometrial hyperplasia involves the abnormal thickening of the endometrium, the lining of the uterus. This condition results from an excess of estrogen without the balancing effects of progesterone, leading to an accumulation of cells in the endometrial lining.
- Types of Endometrial Hyperplasia: There are different classifications of endometrial hyperplasia based on the characteristics of the cell changes. Simple and complex hyperplasia, with or without atypia (abnormal cells), define the severity of the condition and its potential progression to cancer.
The types of cell alterations in your uterine lining determine how medical professionals categorize endometrial hyperplasia. While some endometrial hyperplasia forms significantly raise your risk for cancer, others do not.
Endometrial hyperplasia comes in various forms.
- Endometrial hyperplasia, either simple or complicated (without atypia): This kind of hyperplasia has cells that appear normal and are unlikely to develop into cancer (“without atypia” indicates less likely to develop into cancer). Your doctor might advise hormone treatment, or the condition might get better on its own.
- Atypical endometrial hyperplasia, whether simple or complicated (with atypia): Endometrial hyperplasia that is “atypical” or “with atypia” is more likely to progress to cancer. Your risk of developing uterine or endometrial cancer rises if you don’t get treatment.
Endometrial Hyperplasia of the endometrium is uncommon. 133 out of 100,000 AFAB individuals are estimated to be affected. Those who are approaching or have just finished menopause—the time when a person no longer gets monthly periods—are most likely to experience it.
Symptoms of Endometrial Hyperplasia
- Abnormal Uterine Bleeding: The most common symptom of endometrial hyperplasia is irregular and heavy menstrual bleeding. Women may experience prolonged periods or bleeding between menstrual cycles.
- Pelvic Pain and Discomfort: Some individuals with endometrial hyperplasia may experience pelvic pain or discomfort, although this symptom is less common. Understanding the correlation between pain and the condition is essential for accurate diagnosis.
- Changes in Menstrual Patterns: Endometrial hyperplasia can lead to changes in menstrual patterns, including shorter or longer cycles. Recognizing these variations is crucial for early detection and intervention.
Causes of Endometrial Hyperplasia
Endometrial hyperplasia causes an excess of estrogen and a deficiency of progesterone production. These hormones are necessary for both pregnancy and the menstrual cycle. Progesterone gets your uterus ready for pregnancy, while estrogen thickens your endometrium during ovulation. Infertility results in a decrease in progesterone. Your uterus sheds its lining throughout your menstrual period, which is triggered by the progesterone reduction.
Endometrial hyperplasia patients produce very little if any, progesterone. Your uterus does not lose its endometrial lining as a result. Rather, the lining keeps getting thicker and bigger. The lining’s cells have the potential to develop erratically and closely together.
- Hormonal Imbalance: The primary cause of endometrial hyperplasia is an imbalance between estrogen and progesterone. Estrogen stimulates the growth of the endometrial lining, while progesterone helps regulate and shed it during the menstrual cycle. When there is an excess of estrogen without sufficient progesterone, hyperplasia can occur.
- Obesity and Metabolic Factors: Obesity is a significant risk factor for endometrial hyperplasia, as excess body fat can lead to increased estrogen production. Conditions such as polycystic ovary syndrome (PCOS) and diabetes, which are associated with hormonal imbalances, also contribute to the development of endometrial hyperplasia.
- Reproductive Factors: Nulliparity (never having given birth) and late menopause can increase the risk of endometrial hyperplasia. Pregnancy and childbirth have protective effects on the endometrium, and the hormonal changes associated with menopause play a role in the condition.
Risk factors for Endometrial Hyperplasia
People in perimenopause or menopause are more likely to have endometrial hyperplasia. It rarely occurs in people younger than 35. Other risk factors include:
- Certain breast cancer treatments (tamoxifen).
- Diabetes
- Early age for menstruation or late onset of menopause.
- Family history of ovarian, uterine or colon cancer.
- Gallbladder disease.
- Hormone therapy using only estrogen when you still have a uterus.
- Never being pregnant.
- Obesity.
- Polycystic Ovary Syndrome (PCOS).
- Smoking Cigarettes.
- Thyroid disease.
- Long history of irregular or absent menstruation.
- History of pelvic irradiation (radiation on your pelvis).
- Compromised immune system due to autoimmune disease or medications.
Diagnosing Endometrial Hyperplasia
- Clinical Evaluation: A thorough medical history, including menstrual patterns, reproductive history, and any associated symptoms, is crucial for diagnosing endometrial hyperplasia. Doctors will inquire about risk factors such as obesity, hormonal disorders, and medication use.
- Imaging Studies: Transvaginal ultrasound and pelvic imaging can help visualize the thickness of the endometrial lining and identify any abnormalities. These non-invasive techniques provide valuable information for the diagnostic process.
- Endometrial Biopsy: A definitive diagnosis of endometrial hyperplasia often involves an endometrial biopsy. During this procedure, a small sample of the endometrial tissue is collected and analyzed for cellular changes. Biopsy results help determine the type and severity of hyperplasia.
If the uterine lining is too thick, a biopsy of it will be offered to diagnose the condition. This can be done in the office in most cases. In some cases, however, a procedure, known as dilation and curettage (called a D&C) a portion of the procedure, the cervix is opened, or dilated, to allow the doctor to access the uterus. The doctor then uses a device called a curette to remove of the lining of the uterus. The results may show that the uterine lining cells are:
- normal
- abnormal yet non-cancerous
- abnormal and precancerous
- abnormal and cancerous
Abnormal findings that are non-cancerous and pre-cancerous indicate endometrial hyperplasia.
Management & Treatment
- Hormonal Therapy: Hormonal treatments, such as progestin therapy, aim to balance estrogen and progesterone levels. This can help regulate the menstrual cycle, reduce endometrial thickness, and prevent the progression of hyperplasia.
- Hysterectomy: In cases where endometrial hyperplasia is severe, persistent, or recurrent, a hysterectomy may be recommended. This surgical intervention involves the removal of the uterus and, in some cases, the ovaries.
- Lifestyle Modifications: Lifestyle changes, including weight management, regular exercise, and a healthy diet, play a crucial role in managing endometrial hyperplasia. These modifications can help address underlying factors such as obesity and hormonal imbalances.
How is endometrial hyperplasia treated?
For women with endometrial hyperplasia who have abnormal, non-cancerous cells, progestin therapy may be recommended. This synthetic hormone helps to balance out the effects of estrogen in the system, which should eliminate or minimize symptoms of endometrial hyperplasia.
Women who have not yet reached menopause may be prescribed:
- Birth control pills containing progestin
- Birth control pills containing estrogen plus progestin
- Progestin injections
- Vaginal cream containing progestin
- An intrauterine device (IUD) that gradually releases a progestin (levonorgestrel)
Women who have reached menopause should not take birth control pills containing estrogen plus progestin. They may be prescribed:
- Progestin-only birth control pills
- Progestin injections
- Vaginal cream containing progestin
- An IUD that gradually releases progestin
Importance of Proactive Management
- Preventing Progression to Cancer: While endometrial hyperplasia itself is not cancer, untreated or unmanaged cases can progress to endometrial cancer. Proactive management and timely intervention significantly reduce the risk of malignant transformation.
- Fertility Considerations: For individuals of childbearing age who wish to preserve fertility, hormonal therapies and conservative management options may be explored. It is essential to discuss fertility considerations with healthcare providers to make informed decisions.
- Regular Monitoring and Follow-Up: Continuous monitoring through regular check-ups, imaging, and endometrial biopsies is crucial for individuals with endometrial hyperplasia. This ensures that any changes are promptly identified and addressed.
Conclusion
Endometrial hyperplasia is a condition that requires careful attention, understanding, and proactive management. By recognizing the symptoms, addressing risk factors, and seeking timely medical intervention, individuals can navigate this condition with the guidance of healthcare professionals. Increased awareness, research, and open communication about endometrial hyperplasia contribute to a future where early detection and effective management are commonplace, ensuring the well-being and reproductive health of those affected.
Frequently Asked Questions (FAQs)
-
What are the symptoms of endometrial hyperplasia?
Diagnosis involves a combination of clinical evaluation, imaging studies (transvaginal ultrasound, pelvic imaging), and often an endometrial biopsy. The biopsy helps determine the type and severity of hyperplasia.
-
Are there different types of endometrial hyperplasia?
Yes, endometrial hyperplasia is classified into various types based on the characteristics of cell changes. These include simple and complex hyperplasia, with or without atypia (abnormal cells).
-
How is endometrial hyperplasia diagnosed?
Diagnosis involves a combination of clinical evaluation, imaging studies (transvaginal ultrasound, pelvic imaging), and often an endometrial biopsy. The biopsy helps determine the type and severity of hyperplasia.
-
Can endometrial hyperplasia lead to cancer?
While endometrial hyperplasia itself is not cancer, untreated or unmanaged cases can progress to endometrial cancer. Regular monitoring and appropriate management help prevent this progression.
-
What are the treatment options for endometrial hyperplasia?
Treatment options include hormonal therapy (progestin therapy), hysterectomy (surgical removal of the uterus), and lifestyle modifications. The choice of treatment depends on the severity of hyperplasia, fertility considerations, and individual health factors.
-
Can endometrial hyperplasia affect fertility?
Endometrial hyperplasia can impact fertility, especially in severe cases. However, for individuals of childbearing age who wish to preserve fertility, hormonal therapies and conservative management options may be explored
-
Is there a link between endometrial hyperplasia and obesity?
Yes, obesity is a significant risk factor for endometrial hyperplasia. Excess body fat can lead to increased estrogen production, contributing to the development of this condition.