Placental Abruption During Pregnancy: A Comprehensive Guide
Placental Abruption During Pregnancy: A Comprehensive Guide
Embarking on the journey of pregnancy is a momentous occasion, but it’s essential to understand the potential challenges that may arise along the way. Placental abruption during pregnancy is one such complication that demands attention. This comprehensive guide aims to shed light on what placental abruption entails, its possible causes, symptoms to watch out for, and how it can be managed effectively. By exploring these crucial aspects, expecting mothers and their families can empower themselves with the knowledge to navigate this potential hurdle with confidence and ensure the well-being of both mother and baby.
Introduction
Placental abruption during pregnancy is a topic that warrants attention and understanding for expecting mothers and their families. This unexpected complication can have serious implications for both maternal and fetal health, making it essential to be well-informed. Placental abruption occurs when the placenta separates from the uterine wall prematurely, potentially leading to complications such as hemorrhage and fetal distress. In this comprehensive guide, we will explore the nuances of placental abruption, including its causes, symptoms, diagnosis, and management strategies. By arming ourselves with knowledge, we can better navigate this challenge and prioritize the health and well-being of both mother and baby.
Table of Contents
What is Placental Abruption During Pregnancy?
Placental abruption during pregnancy refers to the premature separation of the placenta from the uterine wall before childbirth. This separation can occur partially or completely and poses significant risks to both maternal and fetal health. The placenta plays a vital role in supplying oxygen and nutrients to the developing fetus, making its detachment a concerning complication. Placental abruption can lead to complications such as hemorrhage, decreased oxygen supply to the fetus, and preterm birth. Understanding the signs and risk factors associated with placental abruption is crucial for early detection and prompt medical intervention, ultimately ensuring the best possible outcome for both mother and baby.
What are the different types of placental abruption?
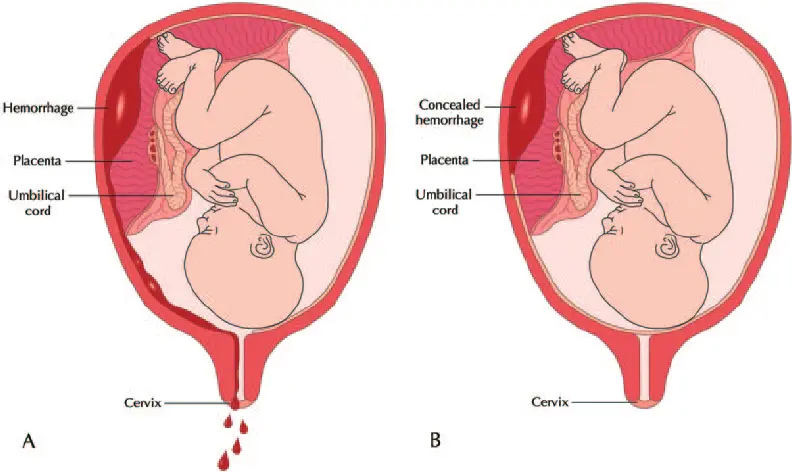
Types of Placental Abruption:
- Complete Placental Abruption: In this type, the placenta separates from the uterine wall, potentially causing severe bleeding and compromising fetal oxygen supply.
- Partial Placental Abruption: Here, only a portion of the placenta detaches from the uterine wall, leading to varying degrees of bleeding and fetal distress depending on the extent of separation.
- Marginal Placental Abruption: This occurs when the placenta partially separates at the edge, resulting in bleeding that may be visible at the cervix.
- Central Placental Abruption: In this type, the separation occurs centrally within the placenta, often leading to significant bleeding and increased risks of complications for both mother and baby.
- Concealed Placental Abruption: Sometimes, the separation may occur behind the placenta, leading to concealed bleeding without visible symptoms, making it challenging to diagnose.
What is the difference between placental abruption and placenta previa?
Placental abruption and placenta previa are distinct pregnancy complications involving the placenta, but they differ in their underlying causes and manifestations. Placental abruption refers to the premature separation of the placenta from the uterine wall, leading to bleeding and potential complications for both mother and baby. In contrast, placenta previa occurs when the placenta partially or completely covers the cervix, increasing the risk of bleeding during labor. While both conditions can cause vaginal bleeding, placental abruption typically presents with abdominal pain and contractions, whereas placenta previa is often asymptomatic until labor, when bleeding occurs.
How common is a placental abruption?
Placental abruption is relatively rare, occurring in about 1 in 100 pregnancies. However, its incidence may increase with certain risk factors, such as advanced maternal age and high blood pressure.
What are the effects of placental abruption during pregnancy?
The effects of placental abruption during pregnancy can vary depending on the severity of the condition and how promptly it is treated. Some potential effects include:
- Maternal Hemorrhage: Placental abruption can lead to significant maternal bleeding, which may require emergency medical intervention to prevent complications such as shock and organ failure.
- Fetal Distress: The separation of the placenta from the uterine wall can compromise the fetus’s oxygen and nutrient supply, leading to fetal distress and potentially affecting its growth and development.
- Preterm Birth: Placental abruption increases the risk of preterm labor and delivery, which can pose additional health challenges for both the baby and the mother.
- Stillbirth: In severe cases, placental abruption may result in fetal demise, particularly if immediate medical attention is not sought.
- Long-Term Complications: In some instances, placental abruption may be associated with long-term health issues for both the mother and the baby, such as developmental delays or neurologic deficits in the child, and an increased risk of future pregnancy complications for the mother.
Symptoms, causes, and risk factors
Symptoms of Placental Abruption:
- Vaginal bleeding, which may vary in severity.
- Abdominal pain or tenderness is often described as intense and continuous.
- Uterine contractions or cramping, potentially accompanied by a sensation of tightening in the abdomen.
- Back pain, which may be sharp or persistent.
- Decreased fetal movement or activity, indicating fetal distress.
Causes of Placental Abruption:
- Trauma or injury to the abdomen, such as from a fall or car accident.
- High blood pressure (hypertension), can weaken the blood vessels in the placenta.
- Smoking or substance abuse, can impair placental function and increase the risk of abruption.
- Maternal age, with older mothers being at higher risk.
- Certain medical conditions, including preeclampsia, blood clotting disorders, and uterine abnormalities.
Risk Factors for Placental Abruption:
- Previous history of placental abruption.
- Maternal age is over 35 years.
- Hypertension, or chronic high blood pressure.
- Smoking or substance abuse.
- Multiple pregnancies (twins, triplets, etc.).
- Uterine fibroids or abnormalities.
- Trauma or injury to the abdomen.
- Preeclampsia or other pregnancy-related complications.
- Certain medical conditions, such as blood clotting disorders or diabetes,.
- In vitro fertilization (IVF) pregnancies may also be at increased risk.
Do you always bleed during a placental abruption during pregnancy?
Bleeding is a hallmark symptom of placental abruption during pregnancy, but it doesn’t always occur. While many cases involve vaginal bleeding, some placental abruptions may be “concealed,” meaning the blood becomes trapped behind the placenta and doesn’t flow out of the body. In these instances, symptoms such as abdominal pain, uterine contractions, and fetal distress may still be present, but there may be no visible bleeding. Pregnant individuals must be aware of all potential symptoms and seek medical attention immediately if they suspect a placental abruption, regardless of bleeding.
What does placental abruption feel like?
Placental abruption can feel like intense abdominal pain or tenderness, often accompanied by persistent back pain. Some describe it as a sharp, continuous sensation, while others may experience uterine contractions or cramping. Additionally, decreased fetal movement or activity may be noticed. However, it’s essential to remember that symptoms can vary, and not all individuals may experience the same sensations during a placental abruption.
What are the first signs of placental abruption?
The first signs of placental abruption may include vaginal bleeding, abdominal pain or tenderness, uterine contractions, back pain, and decreased fetal movement. Immediate medical attention is crucial.
Diagnosis and Tests for Placental Abruption
- Physical Examination: Healthcare providers will perform a comprehensive physical examination, including assessing vital signs, checking for signs of bleeding, and evaluating the abdomen for tenderness or rigidity. This initial assessment helps in identifying potential signs of placental abruption and guiding further diagnostic steps.
- Ultrasound: An ultrasound examination is a crucial diagnostic tool for evaluating the placenta’s location, size, and attachment to the uterine wall. It can also assess fetal well-being by examining the baby’s heart rate and movements. Ultrasound imaging helps determine the extent of placental separation and guides medical management decisions.
- Fetal Monitoring: Continuous fetal monitoring is essential to assess the baby’s heart rate and detect any signs of distress. Electronic fetal monitoring (EFM) involves placing sensors on the mother’s abdomen to monitor the baby’s heart rate and uterine contractions. Changes in fetal heart rate patterns may indicate fetal distress, prompting further evaluation and intervention.
- Blood Tests: Blood tests may be performed to assess maternal blood loss, clotting function, and blood type. Laboratory tests, including complete blood count (CBC), coagulation studies, and blood typing and crossmatching, help determine the extent of maternal hemorrhage and guide appropriate treatment, such as blood transfusions if necessary.
- Magnetic Resonance Imaging (MRI): In some cases, magnetic resonance imaging (MRI) may be utilized to provide detailed images of the placenta and uterus. MRI can offer additional information when ultrasound findings are inconclusive or when there is a need for a more precise anatomical assessment. However, MRI is not routinely performed for diagnosing placental abruption and is typically reserved for specific clinical scenarios.
Grades of Placental Abruption:
Placental abruption is often classified into three grades based on the severity of placental separation and clinical presentation:
- Grade 1: Grade 1 placental abruption is considered mild and involves minimal symptoms. It typically entails less than 20% separation of the placenta from the uterine wall. Symptoms may include mild vaginal bleeding, abdominal discomfort, and subtle changes in fetal heart rate patterns. Grade 1 abruption may not always be immediately apparent, but it requires careful monitoring due to the potential for progression.
- Grade 2: Grade 2 placental abruption is characterized by moderate separation of the placenta, ranging from 20% to 50%. This grade typically presents with more significant symptoms, such as moderate to heavy vaginal bleeding, intense abdominal pain or tenderness, and noticeable changes in fetal heart rate patterns indicative of fetal distress. Grade 2 abruption requires prompt medical attention and may necessitate interventions such as hospitalization and close fetal monitoring.
- Grade 3: Grade 3 placental abruption is the most severe form, involving extensive separation of over 50% of the placenta from the uterine wall. This grade is associated with severe symptoms, including profuse vaginal bleeding, severe abdominal pain or rigidity, and profound fetal distress. Grade 3 abruption poses a significant risk to both maternal and fetal health and requires immediate medical intervention, often necessitating emergency cesarean delivery to mitigate complications and optimize outcomes.
Management and Treatment of Placental Abruption
- Hospitalization: Upon diagnosis of placental abruption, hospitalization is typically recommended for close monitoring and management. Hospitalization allows healthcare providers to closely monitor maternal and fetal well-being and intervene promptly if necessary.
- Intravenous Fluids: Intravenous (IV) fluids may be administered to maintain maternal hydration and stabilize blood pressure. Adequate hydration is essential for supporting maternal circulation and optimizing fetal perfusion.
- Blood Transfusion: In cases of significant maternal hemorrhage, blood transfusions may be necessary to replace lost blood volume and restore hemodynamic stability. Transfusions may include packed red blood cells, fresh frozen plasma, and platelets, as needed.
- Fetal Monitoring: Continuous fetal monitoring is essential to assess the baby’s heart rate and detect signs of distress. Electronic fetal monitoring (EFM) allows healthcare providers to monitor fetal well-being and make timely decisions regarding the need for intervention, such as expedited delivery.
- Cesarean Delivery: In severe cases of placental abruption or fetal distress, prompt delivery via cesarean section may be necessary to mitigate risks to both mother and baby. Cesarean delivery allows for rapid delivery of the baby and minimizes the duration of placental separation, reducing the risk of maternal hemorrhage and fetal compromise.
- Medications: Depending on the clinical scenario, medications may be administered to manage symptoms and optimize maternal and fetal outcomes. These may include tocolytic agents to suppress uterine contractions, corticosteroids to promote fetal lung maturity in preterm births, and medications to support maternal hemodynamic stability.
- Monitoring and Follow-up: Following treatment for placental abruption, ongoing monitoring, and follow-up care are essential to assess maternal recovery and fetal well-being. Maternal vital signs, blood counts, and coagulation parameters should be monitored closely, and fetal growth and development should be assessed through regular prenatal appointments and ultrasound examinations.
- Psychological Support: Placental abruption can be a traumatic experience for expectant mothers and their families. Psychological support and counseling may be beneficial to help individuals cope with the emotional and psychological impact of the condition, address concerns, and facilitate adjustment to the challenges of pregnancy and childbirth.
It’s important to note that management and treatment strategies for placental abruption may vary depending on the severity of the condition, gestational age, maternal-fetal status, and individual patient factors. Healthcare providers will tailor management approaches to each patient’s specific needs and circumstances to optimize outcomes and ensure the best possible care for both mother and baby.
Prevention of Placental Abruption during Pregnancy
While placental abruption cannot always be prevented, certain measures may help reduce the risk or minimize its severity:
- Prenatal Care: Attending regular prenatal appointments allows healthcare providers to monitor maternal and fetal health closely. Early detection and management of conditions such as hypertension, preeclampsia, and placenta previa can help reduce the risk of placental abruption.
- Lifestyle Modifications: Avoiding tobacco smoke, illicit drugs, and excessive alcohol consumption during pregnancy can help protect placental health and reduce the risk of placental abruption. Maintaining a healthy lifestyle with balanced nutrition and regular exercise can also support overall maternal and fetal well-being.
- Managing Chronic Conditions: Managing chronic medical conditions such as hypertension, diabetes, and blood clotting disorders is essential for reducing the risk of placental abruption. Proper management may involve medication, lifestyle modifications, and close monitoring by healthcare providers.
- Trauma Prevention: Taking precautions to avoid abdominal trauma during pregnancy can help minimize the risk of placental abruption. This includes wearing seat belts properly, using safety equipment during recreational activities, and taking measures to prevent falls and accidents.
- Stress Reduction: High levels of stress may increase the risk of placental abruption. Engaging in stress-reduction techniques such as relaxation exercises, meditation, and mindfulness practices may help promote maternal and fetal well-being.
- Prompt Reporting of Symptoms: Educating pregnant individuals about the signs and symptoms of placental abruption and encouraging them to seek immediate medical attention if they experience any concerning symptoms can help facilitate early detection and intervention.
- Obstetric History Review: A thorough review of obstetric history, including any previous occurrences of placental abruption or other pregnancy complications, can help identify individuals at higher risk. Tailored management strategies can then be implemented to optimize maternal and fetal outcomes in subsequent pregnancies.
While these preventive measures may help reduce the risk of placental abruption, it’s important to remember that not all cases can be prevented. Pregnant individuals should work closely with their healthcare providers to address any concerns, manage existing risk factors, and ensure the best possible outcomes for themselves and their babies.

What can I expect if I have a placental abruption?
If you have a placental abruption, you can expect symptoms such as vaginal bleeding, abdominal pain, and possibly fetal distress. Prompt medical attention and treatment are essential for optimal outcomes.
What is my baby’s survival rate after a placental abruption?
The baby’s survival rate after a placental abruption varies depending on factors such as the severity of the abruption, gestational age, and promptness of medical intervention. With timely diagnosis and appropriate treatment, the majority of babies affected by placental abruption can survive, although outcomes may vary.
Can I have another placental abruption?
Yes, it is possible to experience another placental abruption in a subsequent pregnancy, especially if you have risk factors such as a history of placental abruption or certain medical conditions. However, not all individuals will experience recurrent abruptions, and preventive measures may help reduce the risk. Consulting with your healthcare provider is recommended.
When to seek the health care provider
Seek immediate medical attention if you experience symptoms such as vaginal bleeding, abdominal pain, uterine contractions, or decreased fetal movement, as these may indicate a placental abruption requiring urgent evaluation.
Additional common questions (FAQs)
-
Can a baby survive a placental abruption?
How serious these are will depend on how severe the abruption is and how far along you are in your pregnancy. Placental abruption increases the risk of your baby being born prematurely. It may also affect your baby’s growth. Sadly, a very small number of babies do not survive placental abruption and may be stillborn.
-
What causes placenta abruption?
The cause is unknown in most cases, but risk factors may include maternal high blood pressure, abdominal trauma, and substance misuse. Without prompt medical treatment, a severe case of placental abruption can have dire consequences for the mother and her unborn child, including death.
-
Can you have a successful pregnancy after placental abruption?
After placental abruption with perinatal survival in the first delivery, 59% of women had a further delivery, compared with 71% who did not have placental abruption at delivery. After a perinatal loss, the corresponding rates were 83% and 85%, respectively.
-
Can the placenta repair itself?
If the placenta starts separating from the uterus before the baby is born, it is called placental abruption. It can be caused by a medical problem or physical trauma. This quickly becomes life‐threatening for women and babies, and cannot be repaired.
-
What happens to mom after placental abruption?
The immediate risks to the mother, depending on severity, include obstetric hemorrhage, disseminated intravascular coagulation, renal failure, and in rare cases, death. The etiology of abruption is not well understood.
Conclusion
Placental abruption during pregnancy is a serious complication that requires prompt medical attention. By understanding its signs, risk factors, and potential outcomes, expecting mothers can empower themselves to recognize symptoms early and seek timely intervention. While placental abruption cannot always be prevented, proactive prenatal care, lifestyle modifications, and awareness of individual risk factors can help mitigate the risks. With vigilant monitoring, timely diagnosis, and appropriate management, the majority of pregnancies affected by placental abruption can have favorable outcomes for both mother and baby. Open communication with healthcare providers and adherence to recommended guidelines are key to ensuring the best possible outcome.











